In-Home Healthcare for a Person with Pressure Ulcers

What kind of conditions can lead to pressure sores?
Pressure sores, also known as pressure ulcers or bedsores, can develop when the skin and underlying tissues are subjected to prolonged pressure or friction. This pressure can restrict blood flow to the affected area, leading to tissue damage and the formation of a sore. Some of the conditions that may increase the risk of developing pressure sores include:
- Limited mobility or paralysis: Individuals who are confined to a bed or wheelchair and have limited ability to move may be at increased risk of developing pressure sores
- Poor nutrition: A diet that is low in nutrients or calories can weaken the immune system and slow down the healing process, making it more difficult for the body to repair damaged tissues
- Incontinence: Urinary or fecal incontinence can expose the skin to moisture and irritants, which can increase the risk of developing pressure sores
- Neurological conditions: Conditions that affect the nervous system, such as Parkinson's disease, multiple sclerosis, or spinal cord injuries, can affect mobility and increase the risk of developing pressure sores
- Age: As individuals age, their skin becomes thinner and more fragile, which can make it more susceptible to damage
- Medical conditions: Certain medical conditions such as diabetes, peripheral artery disease, or heart failure can affect blood flow and increase the risk of developing pressure sores.
It's important to identify and address any underlying conditions that may increase the risk of developing pressure sores. Additionally, regular monitoring and repositioning can help prevent the development of pressure sores in individuals who are at risk.
How can I support my elderly relative with mobility issues to prevent bed sores?
Here are some tips on how to support your elderly relative with mobility issues to prevent bed sores:
- Change positions frequently: Encourage your relative to change positions often, at least every two hours if possible, to relieve pressure on bony areas. If they are unable to move themselves, you may need to help them or use assistive devices such as a lift
- Use pressure-relieving equipment: Special mattresses, cushions, and pillows can help distribute pressure and reduce the risk of bed sores. Your healthcare provider or a medical equipment supplier can provide recommendations
- Keep skin clean and dry: Keep your relative's skin clean and dry to prevent moisture from causing skin breakdown. Use mild soap and warm water to clean the skin, and pat dry gently
- Moisturise skin: Apply a moisturiser to keep skin soft and supple, which can reduce the risk of skin breakdown. Choose a moisturizer that is fragrance-free and gentle
- Monitor skin for changes: Check your relative's skin regularly for any signs of redness, swelling, or blisters. If you notice any changes, notify their healthcare provider right away
- Encourage activity: Encourage your relative to engage in physical activity as much as possible, even if it's just simple exercises while sitting or lying down. This can help improve circulation and reduce the risk of bed sores
- Ensure adequate nutrition: Proper nutrition is essential for healthy skin. Make sure your relative is getting enough protein, vitamins, and minerals in their diet, and consider talking to their healthcare provider about supplements if necessary.
What causes pressure ulcers?
- Friction: Rubbing or dragging against a surface can cause damage to the skin and make it more susceptible to pressure ulcers
- Shear: When the skin and underlying tissues move in opposite directions, it can cause stretching and tearing of the tissues, leading to pressure ulcers
- Moisture: Prolonged exposure to moisture can soften the skin and make it more prone to damage from pressure
- Poor nutrition: A lack of nutrients can impair the body's ability to repair and maintain healthy skin and tissues
- Reduced mobility: Individuals who are unable to move or change positions frequently are at a higher risk of developing pressure ulcers
- Medical conditions: Certain medical conditions such as diabetes, circulatory problems, and neurological disorders can increase the risk of developing pressure ulcers.
What kind of diet should I give a relative with pressure ulcers?
A healthy, balanced diet is important for everyone, but it is especially important for individuals with pressure ulcers. A diet that is rich in nutrients can help promote wound healing and prevent the development of new pressure ulcers. Here are some general dietary guidelines to follow:
- Protein: Protein is essential for tissue repair and wound healing. Encourage your relative to eat protein-rich foods such as lean meats, fish, poultry, eggs, dairy products, legumes, nuts, and seeds
- Vitamins and minerals: Vitamins and minerals play a crucial role in the healing process. Encourage your relative to eat a variety of fruits, vegetables, and whole grains to ensure they are getting a range of essential vitamins and minerals
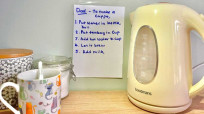
- Fluids: Adequate fluid intake is important to keep the body hydrated and to prevent constipation, which can increase pressure ulcer risk. Encourage your relative to drink plenty of water and other fluids such as fruit juice, milk, and herbal tea
- Caloric intake: Individuals with pressure ulcers may require more calories than usual to promote healing. Consult with a registered dietitian or healthcare provider to determine the appropriate caloric intake for your relative
- Avoid sugar and unhealthy fats: Sugary and fatty foods can impair wound healing and should be limited in the diet. Encourage your relative to choose whole, nutrient-dense foods instead.
My relative won't eat a healthy diet, what can I do?
It can be challenging to encourage a loved one to eat a healthy diet, especially if they have pressure ulcers and may be experiencing pain or discomfort. Here are some tips that may help:
- Talk to your relative about the importance of nutrition: Help your relative understand how nutrition can impact their health and healing. Explain how certain foods can help promote wound healing and prevent the development of new pressure ulcers
- Offer healthy options: Try to offer your relative a variety of healthy, nutrient-dense foods that they enjoy. If they have a favorite food that is not particularly healthy, try to find healthier alternatives that they may enjoy
- Make meals more appealing: Sometimes, presentation can make a big difference. Try to make meals look more appealing by arranging the food in an attractive way or serving it in colorful dishes.
- Consider texture and consistency: Some individuals with pressure ulcers may have difficulty chewing or swallowing, which can make it difficult to eat certain foods. Try to offer foods that are easy to chew and swallow, such as pureed soups or smoothies
- Get creative with flavors: Adding herbs, spices, or other flavorful ingredients to meals can make them more appealing and enjoyable to eat
- Work with a healthcare provider or registered dietitian: If your relative is still resistant to eating a healthy diet, consider consulting with a healthcare provider or registered dietitian. They can provide personalized recommendations and help develop a dietary plan that meets your relative's specific needs and preferences
What services can help me care for a person with pressure ulcers?
- District nursing service: District nurses can provide support and advice on wound care and pressure ulcer management, including dressing changes and positioning
- Tissue viability service: This service provides specialist support for individuals with complex wounds, including pressure ulcers. They can provide advice on wound care and prevention, and may be able to provide specialist equipment such as pressure-relieving mattresses or cushions
- Community occupational therapy service: An occupational therapist can provide advice on positioning, mobility aids, and equipment that can help prevent pressure ulcers from developing or worsening
- Community nursing service: Community nurses can provide wound care and support for individuals with pressure ulcers, including advice on prevention and management.
- Age UK: Age UK offers a range of services for older adults, including advice and support on caring for individuals with pressure ulcers
- Carers UK: Carers UK provides support and advice for individuals who are caring for a loved one with pressure ulcers, including information on financial and legal issues
NHS: The local clinical commissioning group may be able to provide information on local services and resources for pressure ulcer care and management.
What charitable organisations can help me care for a relative with pressure sores?
There are several charitable organisations that can help you care for a relative with pressure sores. Here are some organizations you may want to consider:
- The Tissue Viability Society promotes education and research in tissue viability and wound care. They offer resources and support for healthcare professionals and patients, including a helpline and educational events
- Age UK offers a range of services for older adults, including advice and support on caring for individuals with pressure ulcers
- Carers UK provides support and advice for individuals who are caring for a loved one with pressure ulcers, including information on financial and legal issues
- The Disabled Living Foundation provides information and advice on equipment and products that can help individuals with pressure ulcers, such as pressure-relieving cushions and mattresses
- The National Institute for Health and Care Excellence (NICE): provides guidelines and recommendations on the prevention and management of pressure ulcers. Their website includes resources for healthcare professionals and patients.
It's important to discuss your loved one's specific needs with their GP or a social worker, who can help you identify the most appropriate services and resources for their care.
Next Steps
For more information about caring for a loved one at home join our discussion in our Facebook group Care Begins at Home for ongoing advice and support from our care experts.